Dr. Weeks’ Comment: Again, great anti-aging and cognitive regeneration results from anti-inflammatory agents. Why use a drug when you can eat the most powerful anti-inflammatory food: the seed!
“…An asthma drug has rejuvenated rat brains, making old rats perform as well as young rats in tests of memory and cognition. The drug also encouraged the birth of new brain cells…”
“… As we get older, most of us will experience some kind of brain degeneration. Typically, we lose the ability to make new neurons. Another problem is chronic, low-grade inflammation in the brain, which is implicated in many age-related brain disorders.
To tackle both problems in one go, Ludwig Aigner at Paracelsus Medical University Salzburg in Austria and his colleagues targeted a set of receptors in the brain that, when activated, trigger inflammation...”
(Thanks to Professor Dimitri for sharing this with us.)
23 October 2015
Old rat brains rejuvenated and new neurons grown by asthma drug

It’s as good as new. An asthma drug has rejuvenated rat brains, making old rats perform as well as young rats in tests of memory and cognition. The drug also encouraged the birth of new brain cells.
As we get older, most of us will experience some kind of brain degeneration. Typically, we lose the ability to make new neurons. Another problem is chronic, low-grade inflammation in the brain, which is implicated in many age-related brain disorders.
To tackle both problems in one go, Ludwig Aigner at Paracelsus Medical University Salzburg in Austria and his colleagues targeted a set of receptors in the brain that, when activated, trigger inflammation.
High numbers of these receptors are found in areas of the brain where neurons are born, suggesting they might also be involved in this process, too.
Escape plan
The rats took part in a range of learning and memory tests. One of these, for example, involved the rats being placed in a pool of water with a hidden escape platform. At the start of the study, untreated young rats learned to recognise landmarks and quickly find their way to the platform, while the untreated older animals struggled at the task.
By the end of their six-week drug regime, though, old animals performed as well as their younger companions. “We’ve restored learning and memory 100 per cent, to a level comparable with youth,” says Aigner. He presented his findings last week at the Society for Neuroscience meetingin Chicago.
When the team studied the brains of the animals, they found that old rats that had been given montelukast had 80 per cent less inflammation. They also had an enhanced level of new neuron growth compared with untreated old rats – about 50 per cent of that seen in young rats, says Aigner.
The team also found that the blood-brain barrier – which stops infectious agents reaching the brain and which weakens in old age – was stronger in treated old rats. “Structurally, the brain had rejuvenated,” says Aigner.
No effect on the young
The drug had no effect on young animals, probably because it targets inflammation associated with age and disease, says Aigner. “We’ve identified a target that affects many different systems of the aged and degenerated brain,” he says. “I think the drug reverses the damage associated with ageing.”
Because montelukast is widely used, it should be relatively quick and easy to look for similar effects in clinical trials in people, says James Nicoll, a neuropathologist at the University of Southampton, UK.
Aigner says the results from the rat study are significant enough to warrant a clinical trial. He will start by testing the drug in people with Parkinson’s disease, he says.
“It’s a very promising approach,” says Arthur Roach, director of research and development at charity Parkinson’s UK. “They’ve reversed certain aspects of the aged brain.”
Real ageing
Although the results are in rats, they are exciting because the team used animals that had aged naturally, rather than young rodents with genetic mutations that make them age prematurely, or rodents bred to have age-related disease. “You don’t often see studies in old rats because they’re so expensive,” says Roach.
It is also a promising sign that montelukast can access the brain. “There are a lot of anti-inflammatory drugs out there, but they don’t tend to cross the blood-brain barrier,” says Gary Wenk at Ohio State University in Columbus.
Wenk isn’t surprised that a drug that targets inflammation in the brain should have such “restorative” effects. “It is now becoming accepted that inflammation does lead to neurodegeneration,” he says. Inflammation has also been linked to Alzheimer’s disease and Huntington’s disease, among other conditions.
Bryce Vissel at the Garvan Institute of Medical Research in Sydney, Australia, is cautious. “Millions of people are affected by Alzheimer’s and Parkinson’s worldwide… and hope that science will deliver a cure,” he says. “But so far no promising therapy in an animal model has translated to a therapy in people in neurodegenerative disease.”
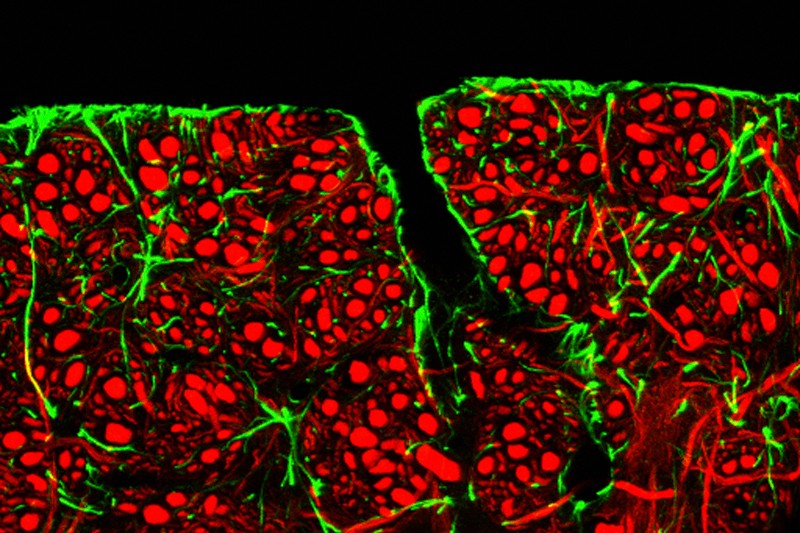
Image information: The blood-brain barrier, credit: C. J. Guerin/MRC Toxicology Unit/SPL
THE ARTICLE
Inhibition of leukotriene receptors boosts neural progenitor proliferation.
Abstract
Neural stem and progenitor cells serve as a reservoir for new neurons in the adult brain throughout lifetime. One of the critical steps determining the net production of new neurons is neural progenitor proliferation, which needs to be tightly controlled. Since inflammation has detrimental effects on neurogenesis and the 5-lipoxygenase/leukotriene pathway is involved in inflammatory processes, we investigated the effects of leukotrienes and montelukast, a small molecule inhibitor of the leukotriene receptors CysLT(1)R and GPR17, on neural stem and progenitor cell proliferation. We demonstrate expression of the leukotriene receptor GPR17 by neural progenitors and by neural stem cells. Stimulation with excess amounts of leukotrienes did not affect progenitor proliferation, whereas blockade of GPR17 with montelukast strongly elevated neural stem and progenitor proliferation, while maintaining their differentiation fate and potential. This effect was associated with increased ERK1/2 phosphorylation suggesting an involvement of the EGF signaling cascade. Based on our results, montelukast and the inhibition of the 5-LOX pathway might be potent candidates for future therapies employing neurogenesis to promote structural and functional improvement in neurodegeneration, neuropsychiatric disease and ageing.
`