Dr. Weeks’ Comment: Cancer STEM cells are on the scene and wrecking havoc in a lethal manner and need to be 1) addressed, 2) doctored (rendered normal “de-differentiated”) – Encourage your doctor and oncologist to get up to speed on the world of cancer STEM cells.
“…Cancer cells acquire invasive and stem cell-like traits by undergoing a process called an epithelial-to-mesenchymal transition (EMT), which transforms cube-like, immobile cells into elongated, mobile ones…”
Seemingly Invincible Cancer STEM cells reveal a Weakness
Fri, 06/06/2014 – 12:55pm

Cancer cells acquire invasive and stem cell-like traits by undergoing a process called an epithelial-to-mesenchymal transition (EMT). Invasive cancer cells, like other mesenchymal cells, move by secreting large scaffolding proteins and other proteins that interact with the extracellular matrix, the structural support that holds neighboring cells together.
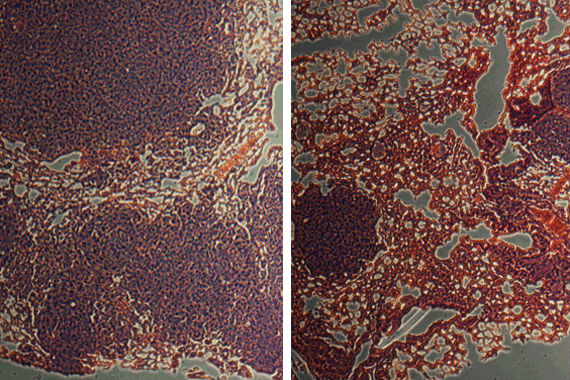
Whitehead Institute researchers have found that pumping out these proteins strains the cancer cells’ ER to their limit. Their work points to one specific part of the process, called the PERK pathway, as being particularly important. When mice were injected with cancer cells treated with a PERK inhibitor, those mice developed significantly smaller and fewer lung tumors (right) than mice injected with untreated cancer cells (left). In these images, tumors are stained dark purple and are surrounded by red lung tissue. (Source: Whitehead Institute/Yuxiong Feng)Metastatic cancer cells, which can migrate from primary tumors to seed new malignancies, have thus far been resistant to the current arsenal of anticancer drugs. Now, however, researchers at Whitehead Institute have identified a critical weakness that actually exploits one of these cells’ apparent strengths””their ability to move and invade tissues.
“This is the first vulnerability of invasive cancer cells that we really understand,” said Whitehead Member Piyush Gupta, whose lab’s latest work is described in the June issue of the journal Cancer Discovery. “For a while we didn’t know if they had any vulnerabilities that could be exploited for therapy. Then, a few years ago we discovered they were exquisitely sensitive to some chemical molecules, and therefore had to have a weakness. But we still didn’t know at the time what that weakness was. Now we know.”
Cancer cells acquire invasive and stem cell-like traits by undergoing a process called an epithelial-to-mesenchymal transition (EMT), which transforms cube-like, immobile cells into elongated, mobile ones. Once mobile, cancer cells can form metastases by using the blood stream as an expressway to distant sites in the body, where they can establish new tumors. In addition to being invasive and metastatic, cancer cells that undergo an EMT are also resistant to radiation and most chemotherapies.
Although they are resistant to most therapies, Gupta and his colleagues had previously identified two compounds with very similar structures that were selectively toxic against the invasive cancer cells that had undergone an EMT, but not their non-invasive counterparts. These unique compounds were discovered in a large screen of over 300,000 chemical compounds.
Intrigued by these compounds that were selectively toxic to metastatic cancer cells, Yuxiong Feng, a postdoctoral researcher in Gupta’s lab, further investigated their activity and discovered that the compounds kill by stressing the endoplasmic reticulum (ER) of EMT cells; non-EMT cells were unscathed because their ER was unaffected by these compounds. Feng also found that other chemicals that cause ER stress also similarly dispatched only the metastatic EMT cells. The obvious question was why these otherwise indestructible cells had such sensitive ERs.
A hint lies at the heart of EMT’s physiology and function. Invasive cancer cells, like other mesenchymal cells, move by secreting large scaffolding proteins and other proteins that interact with the extracellular matrix, the structural support that holds neighboring cells together. Pumping out these proteins strains the cancer cells’ ER to their limit. When Feng treated EMT cells with chemicals that further stressed their ER, the cells died. But when those cells’ production of extracellular matrix proteins was artificially blocked, the cells were much less sensitive to the ER-stressing chemicals.
Feng’s work points to one specific part of the process, called the PERK pathway, as being particularly important. This pathway helps cells survive the stress of secreting copious amounts of proteins, and in EMT cells, it is always active at a low level. In studying roughly 800 patient tumors (both primary and metastatic) across a range of cancer types, including breast, colon, gastric, and lung, Feng found that the expression of EMT genes was tightly correlated with PERK pathway activity. “We’ve found that whenever you have EMT, the PERK pathway is more active,” said Feng, who is the first author of the Cancer Discovery paper. “That means we might be able to use PERK pathway activity as a marker to help guide treatment, since tumors with higher PERK activity would likely be more sensitive to further ER stress.”
As promising as these developments sound, Feng cautions that further work is needed before PERK screening could become mainstay of cancer diagnostics. “Our research provides new insights into the biology and weaknesses of invasive cancer cells. Our findings also raise interesting and important questions for further study: how does the PERK pathway support the malignant function of EMT cells? What is the molecular circuitry activated upon EMT that causes cells to secrete copious amounts of extracellular matrix proteins? It’s all very exciting.”
Source: Whitehead Institute