Dr. Weeks’ Comment: Food is your best medicine as it actually solves the problem rather than just suppressing the symptoms. Anti-inflammatory diets are powerful. SOUL and CORE are anti-inflammatory diets in a packet.
An Anti-inflammatory Diet For Pain Patients
Numerous papers have been published that describe how diet can promote or reduce inflammation, but very few studies have specifically looked at how diet can impact pain syndromes.1-14 In 1991, Kjeldsen-Kragh et al examined how the expression of rheumatoid arthritis would be impacted by a vegetation-based diet.14The outcome was a striking reduction in pain, joint inflammation, and duration of morning stiffness””these benefits were still present at 1-year follow up.
Recently, it has been shown that patients are more likely to suffer with musculoskeletal pains and tendinopathy if they also have metabolic syndrome””which is, in part, treated by adopting anti-inflammatory dietary changes.15-21 In fact, a Mediterranean-style diet has been used to reduce cardiovascular risk factors,22achieve 100% resolution of metabolic syndrome,23 and reduce or resolve non-alcoholic fatty liver disease.24 The ketogenic Mediterranean diet includes olive oil, green vegetables, salads, fish (as the primary protein), lean meat, fowl, eggs, shellfish, cheese, and moderate amounts of red wine.
Regarding pain, a more traditional high-fat ketogenic diet has also been examined. In one animal study, a high-fat paste was fed to rats and within 3 weeks there was a significant reduction in pain and inflammation markers in the animals.25 Multiple anti-nociceptive and anti-inflammatory mechanisms have been proposed to explain this outcome.26
Taken together, these studies support the hypothesis that an anti-inflammatory diet should be applied in pain patients.13 This article will briefly review the chemistry of pain and inflammation and examine various components of the diet, which reduce the expression of pain/inflammation chemistry.
What Is Chronic Inflammation?
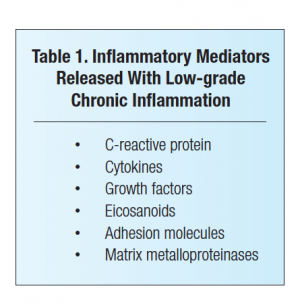
Low-grade chronic inflammation is now known to be a driver of most chronic degenerative diseases.1-14 It is important to understand that low-grade chronic inflammation is not associated with an obvious injury or infection (ie, acute inflammation) and does not predictably resolve.1,2,27 Low-grade chronic inflammation manifests itself both locally and systemically due to the increased cellular release of a variety of inflammatory mediators (Table 1).
These mediators are found to be elevated in seemingly distinct chronic disease such as atherosclerosis28 and osteoarthritis.29 This finding suggests that we should begin to look at chronic diseases as having similar chemical conditions (pro-inflammatory state), which manifest with symptoms that affect particular organs and systems.30
Pain as a Manifestation Of Chronic Inflammation
Multiple cells are involved in the release of inflammatory mediators, which lead to the cellular communication that can generate pain in somatic tissues, such as joint, muscle, disc, ligament, tendon, fascia, or epineurium (Figure 1).31 Nerve cells, especially group IV afferents (sensory C-fibers) and postganglionic sympathetic fibers (motor C-fibers) dominate the innervation of somatic tissues and play an important role in the inflammatory process and tissue homeostasis.29,31-34
Pain researchers describe group IV afferents as having the ability to “taste” the local tissue chemistry, which then, from an operational perspective, leads to their subsequent activation (if the “flavor” is inflammatory), or inhibition, modulation, and/or healing (if the tissue chemistry “flavor” is anti-inflammatory).33 Group IV afferents release a host of mediators, the most well known being substance P. Substance P serves to communicate with local cells by activating cell-signaling molecules, such as nuclear factor κ-B (NF-κB).35 The outcome of substance P stimulation and NF-κB activation is the release of mediators (ie, prostaglandins and cytokines) by the cells, a process that often is referred to as neurogenic inflammation.36 If the mediators released are pro-inflammatory, then inflammation and group IV activation will continue, leading to additional substance P release and the conduction of nociceptive impulses, which lead to pain. In addition to exciting or modulating group IV afferents, the mediators released by local cells will serve to excite or modulate neighboring cells in a paracrine fashion.36 In this context, inflammation and pain necessarily would become chronic, unless local cells release anti-inflammatory mediators.
An interesting fact, as mentioned above, is that cells have the ability to release both pro-inflammatory and anti-inflammatory mediators and in doing so, determine the “flavor” of the tissue chemistry that is “tasted” by group IV afferents. Germane to the topic of this paper, it appears that nutrition is likely a key determining factor that generates the tissue “flavor” of inflammation and, thus, pain expression.
Diet-induced Pro-inflammatory Mediator Release
Multiple factors contribute to chronic “dietary injury,” a term that may be helpful to appreciate how diet can cause chronic inflammation and pain. Dietary injury should be viewed as a cumulative and chronic event, such that monotherapies with nutritional supplements or medications are unable to counteract the multiple “hits” delivered by a pro-inflammatory diet. Table 2 lists the primary sources of dietary injury and their inflammatory consequences.12,37-73 By making unhealthy lifestyle choices, an individual’s body is transformed into a “state” of chronic inflammation. The patient may not feel this transformation until an obvious clinical sign or symptom is present. We now know that stress, lack of sleep, lack of exercise, and inflammatory dietary choices represent types of “non-traumatic” biochemical injury, which causes our cells to generate a low-grade chronic inflammatory state by releasing increased levels of the previously mentioned inflammatory mediators.74-78Diet is most important because the chemistry of the diet is reflected as the chemistry of the cells.
The most obvious dietary example involves the excess consumption of omega-6 (n-6) fatty acids that become part of cell membranes. An excess of n-6 arachidonic acid, a polyunsaturated n-6 fatty acid, is consumed directly from grain-fed animals and farm-raised fish, most notably catfish and tilapia.79,80 Foods processed with oils from corn, safflower, sunflower, and cottonseed contain mostly n-6 linoleic acid, which is converted by the human body into arachidonic acid and incorporated into cell membranes throughout the body.



Editor’s Note: Considerable scientific information and clinical observation have accumulated in recent years showing that chronic pain””particularly the debilitating, severe form requiring opioid treatment””needs a “chronic pain” diet. I have been a proponent of a high-protein diet with avoidance of carbohydrates.1 The fundamental principle of the diet is that patients with chronic pain need to avoid high-glycemic foods (sugars and starches) and eat more protein and vegetables to promote strength, movement, energy, and mental function.
The “anti-inflammatory” diet presented here mirrors many of my personal recommendations, and most experts consider this diet to be healthy. The problem for pain practitioners is that we really don’t know how significant a role inflammation plays in chronic pain states. Consequently, neither this diet nor any others have shown conclusively that pain can be controlled by diet. Despite the lack of “evidence,” Practical Pain Management commends the thoroughness of this article and encourages pain practitioners to advise their patients to eat a healthy diet, exercise, and take supplements, when appropriate.
Reference
1. Tennant F. A diet for patients with chronic pain. Pract Pain Manage. 2011;11(6):22-30.